Cartilage Restoration: Innovative Treatment for Knee Pain in Active Individuals
What is Cartilage?
Articular (or hyaline) cartilage is a tissue in the body that lines the ends of the bones, providing a smooth surface for movement of the joint. It also serves as a shock absorber during activities. When there is an injury to the cartilage in a joint, it does not heal on its own as there is no direct blood supply to aid in this process. Instead, cartilage continues to deteriorate over time, especially with continued activity. This leads to a disease called Osteoarthritis. Fortunately, there are now procedures available to restore the cartilage in a joint without having to go through a joint replacement. The most common joint for a Cartilage Restoration procedure is the knee.
Treatment Options for Cartilage Disorders
There is a spectrum of treatment options for treating cartilage disorders including palliative, reparative, resurfacing, and reconstruction. Palliative treatment is known as Chondral Debridement, where the uneven surface of damaged cartilage is smoothed out during arthroscopic surgery. This does not replace injured cartilage but may relieve pain as there is no longer a loose flap of tissue moving abnormally in the joint. This may be an option for a patient with only a partial thickness cartilage injury or an older patient who does not participate in demanding activities. The recovery time for this procedure is minimal. The patient can be full weight bearing and does not have any range of motion restrictions after surgery.
When there is a very small, focal lesion of missing cartilage, the patient may be a candidate for a reparative procedure known as Marrow Stimulation. This procedure is sometimes referred to as Microfracture. With this procedure, holes are made directly into the lesion allowing bone marrow to escape into the defect. This allows for healing of the lesion with a substance known as Fibrocartilage, which acts similarly to innate articular cartilage when in a small area. This is a simple arthroscopic procedure but does require some restrictions during subsequent rehabilitation to allow the Fibrocartilage to develop and heal.
Cartilage Restoration for Active Individuals
When we think of true “Cartilage Restoration” procedures, there are really two different types – Resurfacing and Reconstruction.
Resurfacing: “Repaving the Street”
When the lesion is too large for microfracture but still only involves the surface of the bone, then a resurfacing procedure is warranted. There are several ways to resurface the end of the bone with new cartilage. One technique is to take the patient’s own unused cells out during an arthroscopic procedure and send them to a lab to be grown into new cartilage cells, which would then be placed over the lesion that is missing cartilage. This process is known as Autologous Chondrocyte Implantation and requires two surgical procedures – one to harvest the cells and another to put them into the defect. The benefits of this procedure are that it uses the patient’s own cells and is able to resurface a large area of damage. The recovery depends on where in the knee these cells are placed, but generally range of motion is encouraged early as cells adhere to the bone and proliferate right away. Patients are able to ride a bike within weeks and even start running after just a few months.
Another resurfacing technique is done by Allograft Implantation. Rather than two separate surgeries, this can be done in one arthroscopic or minimally invasive procedure. The defect is debrided, and the donor cells are pasted into place and fixated with a type of biologic glue. Similarly, patients progressively return to their normal activities within several weeks as the cells grow into real articulating cartilage.
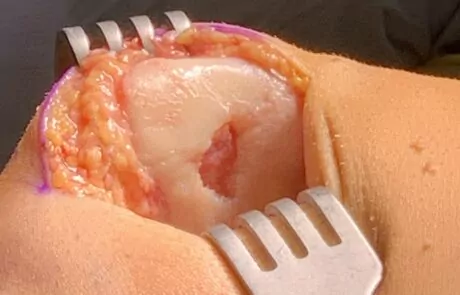
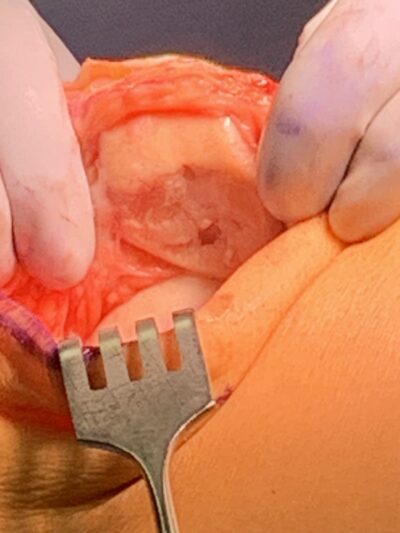
Pre Cartilage Resurfacing Of The Patella
Post Cartilage Resurfacing Of The Patella
Reconstruction: “Filling the Pothole”
When a cartilage defect extends beyond the surface to involve the underlying bone, a structural graft is necessary in a reconstructive procedure to restore the cartilage. The size of the injured cartilage determines whether the cartilage can be obtained from the patient or must come from a donor. If it is a smaller lesion, then a cartilage plug (includes underlying bone) may be taken from a place in the joint that does not need it and placed into the defect. This procedure is called Osteochondral Autograft Transplantation and is typically done with a minimally invasive open incision. However, when the size of the defect is too large to take it from another place, donor tissue is required. In this case, a plug can be made to fit the size of the void after the missing cartilage and damaged underlying bone is removed. Even an oval shaped plug can be fashioned to fill a large, long defect over the weightbearing surface of the knee, which is termed a BioUni. These procedures are called Osteochondral Allograft Transplantations and may be an alternative to partial or total joint replacement for the right patient. Although they do take longer to heal compared to a cartilage resurfacing procedure, the patients generally return to activity within a few months and have excellent outcomes.
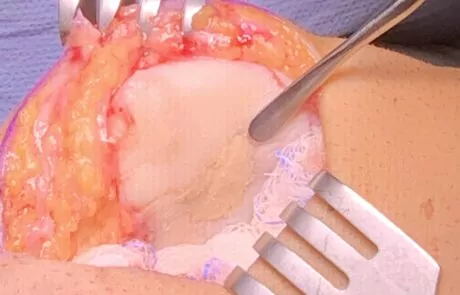
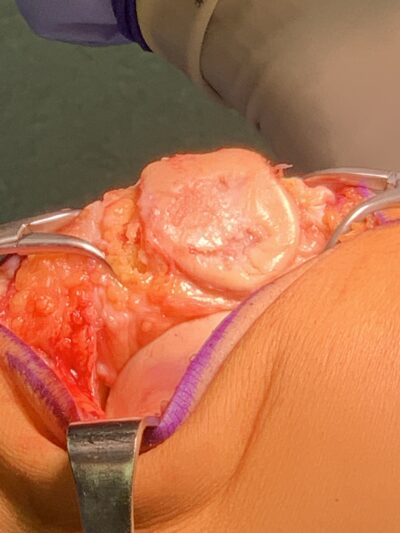
Large Cartilage Defect Of The Medial Femoral Condyle

Cartilage Graft Being Placed Into Defect

Cartilage Graft Placed Into Defect

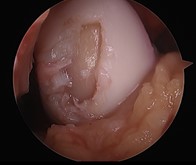
Small Cartilage Defect Of The Medial Femoral Condyle

Large Cartilage Defect Of The Medial Femoral Condyle

Large Cartilage Defect Of The Medial Femoral Condyle
Reconstruction Innovation
There is a very exciting new procedure using the Osteochondral Allograft Transplantation concept to replace the entire undersurface of the patella (kneecap). The patella cartilage is especially vulnerable to injury in athletes, specifically runners. Here in Colorado Springs, we see many patients with this problem who are told that their only options are to stop being active, live with the pain, or get a partial or total knee replacement. This procedure provides an opportunity to restore their cartilage and get them back to activities within a matter of months. We are excited to announce that Dr. Jamie Friedman is the first orthopaedic surgeon to bring this technology to the state of Colorado. The first patient to undergo this procedure here in Colorado Springs is currently doing his physical therapy and has registered to run a marathon this coming June.
Pre Total Biologic Resurfacing Of The Patella
Pre Total Biologic Resurfacing Of The Patella

Donor Patella Ready For Placement
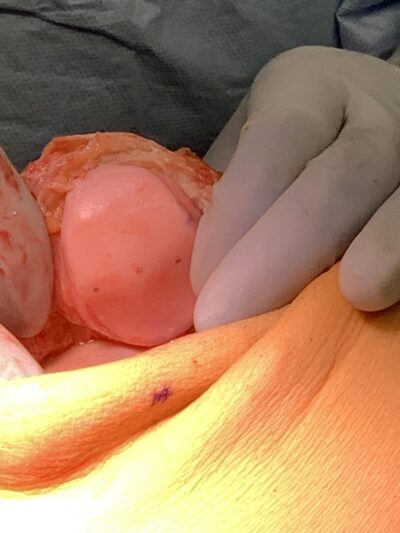
Post Total Biologic Resurfacing Of The Patella
Cartilage Restoration and Joint Deformity: Knocked-Kneed and Bowlegged
Finally, one aspect of Cartilage Restoration that is often overlooked is the alignment of the joint itself. Many people are born either knock-kneed or bowlegged, but if there is too much of this deformity in the joint, it puts additional pressure on one side of the knee. If the underlying problem of leg malalignment isn’t addressed, it can cause continued damage to the existing cartilage and a cartilage restoration procedure may fail. In this case, the patient may be a candidate for realignment surgery to balance out the knee joint in conjunction with restoring the damaged cartilage. If the patient is too knock-kneed (Genu Valgum), then they may need what is called a Distal Femoral Osteotomy. This is when the bottom end of the thigh bone (Femur) is cut and straightened out with an opening wedge. If the patient is too bowlegged (Genu Varum) then they may need what is called a High Tibial Osteotomy. This procedure involves cutting the top end of the shin bone (Tibia) to straighten out the joint with an opening wedge. Although these deformity correction procedures require the longest recovery (several months), they save the patient from a joint replacement and have great long-term outcomes.

Valgus Malalignment Pre Distal Femoral Osteotomy Surgery For Knocked Knee

Valgus Malalignment Post Distal Femoral Osteotomy Surgery For Knocked Knee
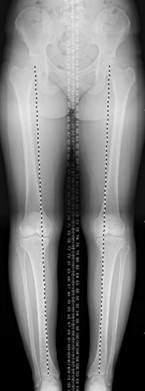
Varus Malalignment Pre High Tibial Osteotomy Surgery For Bow Legged Knee

Varus Malalignment Post High Tibial Osteotomy Surgery For Bow Legged Knee
Is Cartilage Restoration right for you?
So, who is the right candidate for a Cartilage Restoration procedure? The ideal patient is young, active, and motivated. These patients are typically considered too young for a partial or total knee replacement (18-45 years old) and are still involved in an active lifestyle such as team sports, running, hiking, biking, skiing, etc. Patients who currently have pain in their knee with these activities are first assessed in the clinic and with x-ray images. Typically, advanced imaging with an MRI is necessary to fully characterize the cartilage and the underlying bone. If the surgery does not require a donor graft, then the surgical procedure can be scheduled right away. If a donor graft is necessary, then this graft must be ordered, and surgery is not scheduled until a match is found, which usually takes 4-8 weeks.
Cartilage Restoration Recovery
Cartilage Restoration procedures do take some time to recover from – weeks to months – but the patients who are determined to follow the rehabilitation protocols have great outcomes. The goal of Cartilage Restoration is to get patients back to the activities that they love to do without having a joint replacement.
Developed by the Colorado Springs Orthopaedic Group Sports Medicine Team